Definition, terminology
Cholangitis in cats
- inflammation concentrated in the biliary tree (bile ducts), a common form of liver disease, and apparently the second most common after lipidosis. A new simplified classification scheme proposed by the WSAVA Liver Diseases and Pathologies Standards Study Group suggests 3 different forms of cholangitis in cats:
- Neutrophilic (Bacterial) Cholangitis
- Lymphocytic Cholangitis
- Chronic Cholangitis
The new proposed classification scheme also prefers the term "cholangitis" to "cholangiohepatitis" since inflammatory parenchymal lesions are not always present and, if present, are a complication of primary cholangitis.
Neutrophilic (Bacterial) Cholangitis
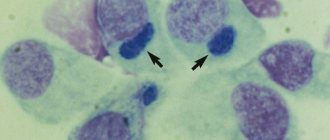
Neutrophilic (bacterial) cholangitis
characterized by the infiltration of large numbers of neutrophils into the hilum of the liver and bile ducts, and is usually associated with ascending bacterial infection, although protozoa are sometimes the cause. The causative agents of feline cholangitis include E. coli, bacteroides, actinomycetes, clostridia and alpha-hemolytic streptococcus. Bile thickening, which can cause partial or complete obstruction of the common bile duct, gallbladder, or intrahepatic bile ducts, often accompanies cholangitis in cats and requires treatment to resolve the cholangitis itself.
Feline neutrophilic cholangitis can be divided into 2 categories:
- spicy
- chronic
Their histological distinction is based on the presence of a large number of plasma cells, lymphocytes, and sometimes macrophages in the chronic stage.
Diagnostics
In either case, inflammation and accompanying tissue swelling interfere with the proper flow of bile, resulting in bile retention in the liver and bile ducts. And since bile is a specific digestive fluid, it can cause significant tissue damage in cases where its normal outflow from the liver is obstructed. Typical signs of cholangiohepatitis in cats include loss of appetite, fever, vomiting, and jaundice (which can cause the sclera of the eyes to become icteric).
Because these clinical signs of feline cholangiohepatitis are similar to those associated with other serious liver diseases such as liver cancer, feline infectious peritonitis, and hepatic lipidosis, a variety of complex diagnostic tests may be required to reach a definitive diagnosis of cholangiohepatitis. In addition to a complete blood count, blood chemistry panel, and urinalysis, these tests may include abdominal x-rays and ultrasounds; bile acid analysis; and a test to determine blood clotting ability. In some cases, an exploratory laparotomy will be necessary to examine the liver and gallbladder. If a preliminary diagnosis of feline cholangiohepatitis is made, a liver biopsy may be performed to confirm the diagnosis. A liver biopsy will also differentiate between types of cholangiohepatitis, an important point since treatment varies depending on the type of cholangiohepatitis diagnosed.
Feline lymphocytic cholangitis
Lymphocytic cholangitis in domestic cats
can be either a late stage of neutrophilic cholangitis or an independent disease. Feline lymphocytic cholangitis is characterized by moderate or severe infiltration of the hepatic hilum area with small lymphocytes ± hyperplasia of the bile ducts, portal or periductal fibrosis. Feline diseases often associated with lymphocytic cholangitis include inflammatory bowel disease and pancreatitis. Inflammatory bowel disease can lead to retrograde passage of bacteria into the common bile duct, leading to pancreatitis and cholangitis. It is important that despite severe inflammation in the small intestine, cats with cholangitis will not always have diarrhea.
Chronic cholangitis in cats
Chronic cholangitis associated with infestation of liver flukes (Amphimerus pseudofelineus, Platynosomum concinnum, etc.)
is a 3rd form of cholangitis. Chronic cholangitis in cats secondary to fluke infestation is characterized by severe bile duct ectasia, moderate to severe ductal epithelial hyperplasia, severe concentric periductal fibrosis, and sometimes adult flukes and/or eggs may be found within the bile duct lumen.
Cholangiohepatitis in a cat
When the bile ducts and liver become inflamed, cholangiohepatitis occurs in cats. The disease has an acute and chronic course and is accompanied by vomiting, jaundice of the mucous membranes, and hyperthermia. If the pet's health deteriorates, the owner is obliged to show it to a veterinarian, who will conduct a diagnosis, prescribe medications and nutritional therapy, which determines the prognosis.
Based on their practice, veterinarians are confident that cholangiohepatitis can provoke irreversible processes in the liver, such as cirrhosis.
Clinical signs of cholangitis in cats
Clinical signs of cholangitis in cats associated with inflammatory liver disease are variable and nonspecific, and are sometimes the same as those seen in hepatic lipidosis. Partial or complete anorexia is more common, and sometimes this is the only symptom. Other less common symptoms include weight loss, lethargy, vomiting, diarrhea and fever. Cats that develop acute cholangitis are younger (mean age 3 years) than cats with chronic cholangitis (mean age 9 years) or hepatic lipidosis (mean age 6.2 years). Males are more susceptible to acute neutrophilic cholangitis. Cats with acute cholangitis are more severely ill than cats with other liver diseases.
Prognosis of cholangiohepatitis in cats
In general, the prognosis of cholangiohepatitis in cats is unpredictable. If diagnosed early in the disease, some cats with the suppurative form of the disorder may respond well to antibiotic therapy and eventually return to normal. And long-term remission is possible in cats that are effectively treated for the refractory type. However, the prognosis is poor for cats diagnosed with any type of cholangiohepatitis when it has already reached a more advanced stage. Severe cholangiohepatitis can progress to biliary cirrhosis, in which vital bile duct tissue is replaced by tough connective tissue. Although biliary cirrhosis is considered the final stage of severe cholangiohepatitis, it is rarely seen because cats with severe disease and those misdiagnosed rarely live long enough to develop it. Prompt diagnosis and treatment will increase the likelihood that treatment will be successful.
Diagnosis of cholangitis in cats
Laboratory findings will show moderate to marked increases in serum bilirubin, alkaline phosphatase, and ALT.
Most cats with acute or chronic cholangitis do not have detectable changes in the echogenicity of the hepatic parenchyma. Conversely, cats with hepatic lipidosis will show diffusely hyperechoic parenchyma. Pathologies of the bile ducts can be visible with cholangitis. These pathologies include distension of the gallbladder and/or common bile duct, cholelithiasis, cholecystitis and bile stagnation. The common bile duct usually appears as an anechoic, tubular, tortuous structure, 2 to 4 mm in diameter with an echogenic wall. Distension of the gallbladder and common bile duct (ie, greater than 5 mm in diameter) occurs as a result of cholecystitis or duct obstruction. The wall of the gallbladder may become thickened due to inflammation or swelling. Definitive diagnosis requires taking a liver biopsy for histological examination, of course after coagulation tests. Cultures of bile and/or liver parenchyma should be done if possible.
Cholangiohepatitis in cats
Cholangiohepatitis
is an inflammation of the liver and bile ducts.
The wide prevalence of cholangiohepatitis in cats is associated with the peculiarities of their anatomy: the pancreatic duct and the gallbladder ducts connect before emptying into the duodenum. Therefore, inflammation of the small intestine or pancreatitis
(inflammation of the pancreas) also leads to inflammation of the bile ducts (
cholangitis
).
Cholangiohepatitis can manifest itself in acute and chronic forms.
Acute form
occurs more often in young cats.
It begins with a sudden refusal to feed and lethargy. Vomiting appears, body temperature often rises, and the abdominal area is painful. With acute hepatitis, dehydration quickly occurs. After this, the so-called “jaundice” or icterus
(yellowish tint of the skin and mucous membranes), which is noticeable on the sclera of the eyes and gums. During this period, the activity of liver enzymes, bilirubin and the number of leukocytes in the animal’s blood increases.
Chronic form
Cholangiohepatitis is more common than acute, and older cats are more prone to it. Symptoms with this course appear and disappear in periods, with periods of exacerbation often associated with stress.
Depending on the type of cells that are found during microscopy of liver samples, chronic cholangiohepatitis may have different names. If lymphocytes predominate, it is called lymphocytic cholangiohepatitis
;
if neutrophils - then neutrophilic
;
if other defense cells (macrophages, plasmacytes) – then granulomatous
.
All forms of cholangiohepatitis can ultimately lead to liver atrophy ( cirrhosis)
).
The causes of acute cholangiohepatitis are often bacterial infections that pass to the liver from the small intestine (duodenum) and pancreas. In addition, acute cholangiohepatitis can be caused by coronavirus infection, intoxication, or feeding with low-quality or unbalanced feed.
Among the causes of chronic cholangiohepatitis, genetic predisposition comes first; it can also be due to an autoimmune disease, helminthiasis, cystoisosporosis, or malnutrition.
- Hepatic lipidosis
. Cats do not tolerate periods of not eating well (anorexia). At this time, their liver often begins to store fat, which leads to lipidosis; the functional liver tissue is irreversibly replaced by fatty tissue. Cats with a lack of appetite due to cholangiohepatitis are at risk. - Hepatic encephalopathy
. Due to increased levels of ammonia and other unwanted components in the blood, brain damage occurs. - Portal hypertension
and the formation of free fluid in the abdominal cavity (ascites). - Sometimes chronic cholangiohepatitis progresses to cancer. In humans, there has been a proven connection between chronic stimulation of lymphocytes and the occurrence of malignant lymphoma. Therefore, it is likely that chronic lymphocytic cholangiohepatitis in cats can provoke lymphoma and malignant abnormalities of lymphocytes.
- General clinical examination of the animal.
- General clinical and biochemical blood test. The presence of hepatitis or chronic inflammation of the intestines and pancreas is indicated by a high level of GGT, an increase in ALT and alkaline phosphatase with normal levels of thyroid hormones. The level of bilirubin and globulins also increases, cobalamin and folic acid decrease.
- Serological studies. Used for suspected viral infections (feline leukemia, feline immunodeficiency, feline viral peritonitis), as well as toxoplasmosis.
- X-ray examination.
- Ultrasound of the abdominal cavity (is important in diagnosing cholangiohepatitis or obstruction (blockage) of the bile duct).
- Liver biopsy. A needle is inserted through the abdominal wall into the animal's liver and material is collected for further research. The best way to diagnose hepatitis is by examining small pieces of the animal's liver. They are obtained by exploratory laparotomy (surgically) or by biopsy. Both procedures pose a certain risk and must be carried out with extreme caution, because in severe cases of the disease, the affected organs may bleed during puncture, and anesthesia poses a risk to the sick animal.
- Bacterial culture of liver and bile. If liver and bile samples can be obtained for pathological examination, it may be possible to test them for the presence of bacteria.
- stabilization of the body's condition in critical cases (intravenous therapy with electrolyte solutions). If necessary, artificial or parenteral nutrition and antiemetics are prescribed;
- antibiotics;
- choleretics and hydrocholeretics (substances that help the passage of bile from the liver to the intestines). They are prescribed to prevent bile stagnation, because this is one of the main phenomena of cholangiohepatitis;
- anti-inflammatory drugs;
- immunosuppressants (prescribed for lymphocytic portal hepatitis);
- vitamins K, E, B12. With cholangiohepatitis, the ability to absorb these vitamins through the intestines is reduced. In some cases, the use of taurine, folic acid and L-carnitine is also indicated.
The cat should be switched to a diet containing a reduced amount of sodium, carbohydrates and an increased amount of protein. It is not advisable to feed your animal food containing sucrose or fructose.
To avoid hepatic encephalopathy, if the level of ammonia in the blood of a particular animal is elevated, the amount of protein in its diet should be limited, because Protein is the main source of ammonia in the body. It is very important to feed your cat small meals multiple times throughout the day.
Therapy for cholangitis in cats
Specific treatment for cats with cholangitis
based on the results of a liver biopsy. Neutrophilic cholangitis in cats is treated with antibiotics. The antibiotics of choice should be excreted into the bile in an active form and should be active against aerobic and anaerobic coliform bacteria. Tetracycline, ampicillin, amoxicillin, erythromycin, chloramphenicol and metronidazole are excreted in active form; however, some of them have serious side effects. Erythromycin is not active against gram-negative bacteria, tetracycline is hepatotoxic, and chloramphenicol can cause anorexia. As a result, ampicillin or ampicillin with clavulanic acid is most often used for treatment. These drugs can be combined with enrofloxacin to expand the spectrum of action. Treatment for 2 months or more is recommended. Cats with lymphocytic cholangitis are usually treated with immunomodulatory therapy, including a combination of prednisolone and chlorambucil.
Choleretic drugs such as ursodeoxycholic acid (Actigall, Ursofalk) are recommended for any inflammatory diseases of the liver of cats. It has anti-inflammatory, immunomodulatory and antifibrotic properties, and also increases the fluidity and secretion of bile. Ursodeoxycholic acid can be given to cats at a dose of 10-15 mg/kg every 24 hours orally. Denamarin (adenosylmethionine, a type of our heptral) can be used as an antioxidant to reduce damage to hepatocytes. If hemorrhagic diathesis develops, injections of vitamin K1 (5 mg/cat every 1-2 days subcutaneously) are indicated. Nutritional support is of great importance for a cat with cholangitis, and esophagostomy placement is often necessary. Surgical intervention is recommended if choleliths are detected or if there is obstruction of the common bile duct. If complete extrahepatic bile duct obstruction is detected, surgical decompression is performed and a bile-intestinal anastomosis is performed (ie, cholecystoduodenostomy or cholecystojejunostomy).
Good to know
- Histopathological changes in small animal hepatobiliary diseases
- Clinical characteristics of hepatocellular carcinoma
- Clostridium perfringens and Clostridium difficile in dogs and cats
- Giardia duodenalis and Cryptosporidium spp. humans from domestic dogs
- Platynosomum fastosum infection in outdoor cats
- Complex cholangitis/chonlangiohepatitis in cats against the background of Platynosomum fastosum infestation
- Histopathological features, immunophenotyping, cloning and eubacterial fluorescence in situ hybridization in cats with lymphocytic cholangitis/cholangiohepatitis
- Differentiating benign and malignant causes of lymphocytosis in the bone marrow
- Prognostic markers of hepatic lipidosis in cats: a retrospective study of cats
- Pancreatitis and diabetes mellitus in cats