Corneal ulcers in cats are often caused by trauma or burns. This is an extremely dangerous disease that develops rapidly and leads to complete blindness. Therefore, it is important to consult a veterinarian in time. Therapy is carried out depending on the degree of eye damage. Medicines and surgery are used. In the worst case, the diseased eye is completely removed.
General information
A corneal ulcer in a kitten is one of the most common and dangerous eye diseases that occurs in cats. This is an inflammatory process that is accompanied by destruction of eye tissue (epithelium, stroma and Dessemet membranes). Damage varies in diameter and depth. Depending on the degree of damage, the following types of ulcers are distinguished, which are listed in the table:
| Name | Description |
| Superficial | Damage to the upper layers of the stroma |
| Deep | Corrodes most of the second level of the cornea |
| Descemetocoeli | Affects the membrane |
| Through | Destruction of the entire cornea |
Diagnostics
Diagnostic procedures are similar in cats and dogs. The veterinarian examines all external elements of the eye apparatus: cornea, conjunctiva, eyelids (including the third). Magnifying glasses are used to determine the shape and depth of ulcers. Next, the corneal reflexes and reaction to light are assessed.
A fluorescein test is mandatory, in which the damaged areas acquire a characteristic color. This method allows for differential diagnosis with other red eye diseases (uveitis, glaucoma, conjunctivitis).
If purulent discharge is detected, a bacterial study of the exudate is prescribed to identify the pathogen and determine sensitivity to antibiotics. Additionally, a Schirmer tear test and cytological analysis may be required.
Causes
The following types of ulcers are distinguished by origin:
Such formation may be of a dystrophic nature.
- inflammatory;
- bacterial;
- dystrophic;
- neurogenic;
- xerotic;
- traumatic.
Animals that belong to brachycephalic breeds are more susceptible to ulcers. That is, animals with shortened muzzles (Persians, British, Himalayan).
This is due to the specific location of their eyes. In such individuals, the secretion of tear fluid is more often impaired, which also affects the progression of the pathology. Often, corneal erosion begins to develop after injury to the visual apparatus. Another common cause is exposure to chemicals on the eyes. This causes a burn, which leads to destruction of the cornea.
Viral and bacterial sources of infection are less common. Thus, infection with keratitis, herpes or rhinotracheitis without treatment turns into an ulcer and leads to destruction of the cornea. The eyes are often affected by staphylococcus and streptococcus bacteria. Another source of disease is the entroion. This is a disease in which the ligaments of the eye relax and the eyelid turns inward. Because of this, the cornea is damaged and inflammation begins.
The disease can develop after the animal has suffered conjunctivitis.
Causes of ulcer development:
- conjunctivitis;
- trigeminal nerve injury;
- deterioration of blood circulation;
- dry eye syndrome.
A few words about the disease
Before we begin to describe the symptoms and causes of the formation of ulcers on the cornea, let us dwell in more detail on the structure of the cornea itself in order to better understand the danger of its ulceration. So, the cornea is a membrane that covers the eyeball and thereby protects it from the external environment. In a sense, this membrane can be compared to glass.
The cornea itself consists of three layers:
- the top layer consists of epithelium - it is extremely thin and therefore completely invisible to the naked eye;
- in the middle is the stroma, which is the core of the cornea, its backbone;
- the bottom layer is Dessemet's membrane. His ulcers are the last to strike.
Most diseases affecting the cornea result in clouding of the cornea.
An ulcer occurs as a result of the fact that the surface epithelium literally grows into the deeper layers of the cornea, thereby violating their boundaries and leading to damage. The ulceration is considered severe even when it reaches the stroma. With this course of the disease, veterinarians prefer to prescribe surgery to be sure of the success of subsequent treatment.
Appearance of blood vessels
Ulceration is sometimes accompanied by the appearance of blood vessels in the cornea that are absent in a healthy eye. Such vessels appear in the most severe cases of corneal damage and indicate that the ulcers have penetrated quite deeply. The vessels originate in the sclera and rush directly to the site of the ulcer.
When an ulceration occurs, the cornea becomes covered with blood vessels, preventing it from healing.
The problem with the appearance of blood vessels is that they are in no hurry to disappear even after successful healing of corneal ulcers, preventing the animal from regaining its previous good vision. Such vessels are destroyed by introducing corticosteroids into the cat’s body, which are prescribed only after all ulcers have completely healed.
Types of corneal lesions
In total, there are two types of corneal lesions, differing in the depth of spread of the ulcers.
Table 1. Types of corneal ulcers
| Type of lesion | Affected area | Description |
| Medium depth | Stroma | When the stroma is damaged, a large amount of intercellular fluid leaks into it, which leads to clouding of the cornea and potentially threatens the pet with partial loss of vision |
| Deep | Dessemet membrane | When the ulcers sink even deeper, to the very base of the cornea, we are talking about descemetocele. In the worst case scenario, Dessemet's membrane can rupture under the influence of ulcers, which will lead to flooding of the eyeball with intercellular fluid |
| Perforated | Base of the eyeball | Penetrates most deeply, which occurs quite sharply. There is only one method of dealing with a perforated ulcer - removing the eyeball |
Diagnostic methods
The presence of a formation in the organ is confirmed during a biomicroscopic examination.
It is impossible to determine the stage of the disease only by external examination of the cat’s visual apparatus. To detect the presence of an ulcer, biomicroscopy is performed. A slit lamp is used to determine the depth of the lesion. To more accurately determine the area of inflammation, fluorescein is used. Once on the surface of the organ, the liquid turns the areas damaged by the ulcer green. The level of damage can also be determined using ultrasound. To identify the root cause of inflammation, a Shimmer test is done. Be sure to measure the fundus and the amount of tear fluid.
Treatment
Treatment of corneal ulcers largely depends on the severity of the disease and the depth to which the ulcers have reached. If domestic cats are expected to be seen by a veterinarian at the initial stage of ulceration, then conservative treatment is prescribed. If the animal comes to the doctor in a neglected state, then surgery may be prescribed.
A veterinarian can determine an effective treatment method only after a detailed examination of the animal’s eyes.
The most superficial and small ulcers disappear within a week. If the ulcer reaches Descemet's membrane and a descemetocele occurs, then even the most competent treatment risks not yielding positive results. The owner of the animal must immediately keep in mind that the deeper the ulcers spread, the more expensive it will cost him to treat the animal.
Treatment of pathology
Due to the fact that corneal ulcers in cats progress rapidly, it is necessary to prescribe therapy in the first days after diagnosing the pathology. If the veterinarian has identified a mild degree of damage, then therapy is carried out using conservative methods. In more serious cases, urgent surgery is required. According to the Eye Research Institute, the cause of the ulcer should be treated first, not its symptoms.
Operating method
Serious damage to this eye membrane in an animal can only be cured surgically.
Prescribed only for deep ulcerative lesions. If a cat has an accumulation of pus, constriction of the pupils or melting of the cornea, then surgery is the only way out to preserve vision. This method is necessary if a foreign body (chips, eyelashes) gets into the cat’s eye. All treatment takes place under general anesthesia. The doctor cleans the affected areas of dead tissue, and then the incisions are closed with a patch (tissue from the conjunctiva, donor materials). An artificial cornea is often used and implanted into the animal's eye.
The stitches are removed after 2 weeks, but a scar forms in their place. During the postoperative recovery period, a special collar is put on the cat, which protects the eye from damage and scratching. A course of antibiotics is also prescribed to maintain health. Adequate nutrition is a must.
Medication method
To remove inflammation, doctors prescribe a course of eye drops and ointments. The products are used 5-6 times a day. For best effect, ointments are applied at night. Antibacterial drugs are used: “Tsiprolet”, “Iris”, “Levomycetin”. If the cause of the ulcer is a virus, then the following medications are used: Tobrex, Idoxuridine, Trifluridine. Streptomycin and Tetracycline are widely used.
Fosprenil will support the animal’s immunity during such a serious illness.
Antibiotics are given orally or through injections. To support the body, immunostimulants are used (Roncoleukin, Fosprenil, Gamavit, Anandin). In addition, the veterinarian prescribes anti-inflammatory and antibacterial medications. If all these remedies do not help, then they move on to the surgical method of treatment.
Infected ulcers
The absence of corneal epithelium deprives the stroma of its natural barrier to infection by bacteria that are usually found in the conjunctival sac (fungal infection is rarely found in infected corneal ulcers in pets). The action of bacteria and host enzymes deepens the ulcers, which begin to destroy the stroma. If the bacterial infection is not treated, corneal perforation may result as the ulcer progresses.
Diagnosis Infection of corneal ulcers should be suspected if the ulcers do not heal after a certain time, and even more so if they enlarge. A yellow or white appearance of the cornea suggests leukocyte infiltration, which is an indicator of infection. The swollen or jelly-like appearance of the cornea is caused by the action of collagenase, which dissolves the stroma, and is characteristic, but not indicative, of a Pseudomonas infection. Animals with infected corneal ulcers should be admitted to the hospital and monitored frequently until the infection is controlled or treated surgically.
If infection is suspected, a small spatula is used to collect samples of the affected cornea for culture, cytology, and antibiotic sensitivity testing. Smears are stained with Wright-Giemsa to identify the basic morphology of bacteria: most gram-positive microorganisms are cocci, and most gram-negative microorganisms are rods. The most common species found in infected corneal ulcers in dogs are Staphylococcus, Streptococcus, and Pseudomonas, which are resistant to most antibiotics.
Treatment (see Table 1).
Drug Treatment Antibiotic treatment of suspected infected corneal ulcers should be based on the results of diagnostic tests. If cytology shows the presence of gram-negative bacteria, drugs effective against Pseudomonas spp should be used, such as a topical ciloxan solution (0.3% ciprofloxacin solution, Alcori) or tobramycin (0.3% tobramycin solution, BauschandLomb). If cocci are found, then use a triple solution of antibiotics (neomycin/polymyxin/gramicidin). Antibiotic solutions are used sequentially with a 2-3 minute interval between instillation of each solution. The interval between applications should be less than 6 hours; to sterilize ulcers, it is advisable to instill antibiotics every 2 hours.
Cycloplegic drugs and analgesics. These animals will have much more pain than patients with uninfected ulcers. Topical atropine with adequate frequency of instillation to maintain mydriasis (every 8-12 hours) will help here. Taking oral aspirin will also help relieve pain.
Topical serum. Peeling of corneal ulcers is the result of host and bacterial proteases that degrade collagen. The serum contains a large amount of protease inhibitors, therefore, treatment of corneal ulcers with serum can slow down the destruction of collagen. The serum is instilled at the same frequency as antibiotic solutions.
Surgery Surgery is indicated when the ulcer extends to one-half to two-thirds of the stromal depth or progresses despite aggressive treatment.
Creation of a conjunctival flap is the only surgical treatment option because it becomes the only source of fibrovascular infiltrate for the thinning cornea. An additional advantage of the conjunctival flap is the antibacterial and anti-collagenase effect of leukocytes and plasma. Aggressive antibacterial treatment is indicated before placing a conjunctival flap, because if the flap site becomes completely infected, the cornea will reject it. Proper placement of a conjunctival flap requires extensive experience and should be performed by a veterinarian skilled in corneal surgery techniques, ideally a professional ophthalmologist.
Corneoscleral transposition surgery is an alternative procedure for repairing corneal defects. In this procedure, the healthy cornea and sclera adjacent to the ulcer are mobilized and moved to close the defect. This procedure has no advantage over the creation of a conjunctival flap. This procedure also requires experience and special tools to perform this procedure satisfactorily.
The use of ophthalmic cyanoacrylate is another treatment option for deep corneal ulcers. Cyanoacrylate adhesives have an antibacterial effect, but are not able to supply nutrients to the diseased cornea like a conjunctival flap or corneoscleral transposition. Before applying cyanoacrylate, the cornea must be dried and a small amount of adhesive placed on the wound. If there is no competent ophthalmological surgeon or there is no money for the operation to create a conjunctival flap, then the application of glue is provided for the treatment of deep ulcers.
There is no point in treating deep, infected corneal ulcers with a third eyelid flap because it will prevent drugs from penetrating the infected ulcer. If the veterinarian wants to close a corneal ulcer, it is better to use temporal tarsorrhaphy rather than creating a third eyelid flap. The drugs are administered through the medial part of the canthus, where nothing prevents their passage into the ulcer. Moreover, with temporal tarsorrhaphy, one can partially see the ulcer, which is not possible when creating a third eyelid flap. Mattress sutures are placed over the defect and tied in a bow so that the doctor can later loosen the sutures, check the ulcer, and then pull the sutures back.
Therapeutic techniques
Therapy depends on the form and severity of the disease. So, if you have a descemetocele, it will be much longer, more expensive, and no one will give you any special guarantee of a cure. In mild cases, provided treatment is started in a timely manner, small lesions can heal within a week. To prevent bacterial contamination of ulcer surfaces, antibiotics and other antimicrobial agents may be prescribed. Sedatives are mandatory (we have already indicated that the pathology is very painful).
Please note that antibiotics and painkillers applied to the cornea in the form of drops remain effective for a maximum of four to five hours (then the medicine is simply washed off). Therefore, it is necessary to “dig” your pet more often. If you do not have the opportunity to drop medications into your cat's eyes every hour, it is better to use ointments. They are washed off much less easily, and therefore the effectiveness of the applied drug lasts much longer.
We have already mentioned that in cats with corneal ulcers, any movement causes pain for centuries, which is why the animals constantly sit with their eyes tightly closed. To alleviate this condition, experts prescribe atropine. Please note that this drug, although it relieves pain and muscle spasms, greatly dilates the pupil. This means that during the treatment period the animal becomes a kind of “vampire”, extremely sensitive to any light. It must also be remembered that the pupil, even after the end of treatment, does not return to its normal state immediately, but after a few days.
For best results, antibiotics should be used every four to six hours. On the other hand, with the additional prescription of atropine (to relieve spasm of the eye muscles), it must be administered no more than twice a day (usually once every two days).
If the ulcerative lesion is already deep enough, and there is a suspicion of descemetocele, all measures should be taken to speed up healing. It should be taken into account that for some reason cats are not happy with blindfolds, and therefore it is necessary to prevent eye licking in other ways. In severe cases, you not only have to put a surgical collar on the cat, but even sew up the eyelids for two or three days!
The worst thing is when a large number of dead cells accumulate along the edges of the ulcer, which hinders the normal healing process. In such cases, a surgical operation is indicated, during which a specialist will remove these tissues. Of course, this surgical intervention is performed exclusively under general anesthesia. Fortunately, in practice, treatment without surgery is more common, but it shows good results only in cases where the owners consulted a veterinarian in time!
Corneal ulcer
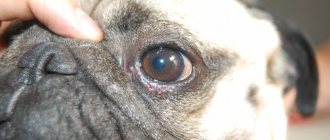
Corneal ulcer is an inflammation of the cornea, accompanied by necrosis of the epithelium and stroma with the formation of a defect. The disease is typical for dog breeds that have natural exophthalmos: French bulldog, Pekingese, etc. Of the cat breeds, Persian cats suffer more often than other breeds.
Corneal erosion is inflammation of the cornea with disruption of the epithelial layer.
It is not always possible to clinically distinguish between ulcers and corneal erosions, therefore these pathological processes are combined with the term “ulcerative keratitis.”
As a result of external influence on the cornea, an inflammatory process occurs, followed by the formation of an ulcer. It can be superficial or deep, complicated or uncomplicated. A superficial ulcer spreads to the epithelium and upper layers of the corneal substance (stroma).
A deep ulcer penetrates the entire thickness of the stroma. If it spreads to the posterior limiting plate (Descemet's membrane), perforation of the anterior membrane of the eye is possible.
| Ulcerative keratitis (Persian cat) |
The formation of a focus of epithelial loss in the cornea stimulates the migration and proliferation of epithelial cells, resulting in complete closure of the defect after 5-7 days. Healing of a corneal stroma defect is a more complex and lengthy process. Relatively superficial ulcers close by migration and proliferation of the epithelium. However, in most cases, ulcers that spread to the deep layers of the corneal substance heal with the help of connective tissue within a few weeks. In this case, purulent complications often develop.
A disease of the epithelial basement membrane, in which the connection of the regenerating epithelium with the underlying stroma is disrupted, slows down the healing of the ulcer.
As a result, slow-healing ulcerative keratitis, refractory to treatment, develops. Causes of ulcerative keratitis: eye injury (closed or penetrating); diseases of the eye appendages (distichiasis, ectopia of eyelashes, inversion and eversion of the eyelid, trichiasis, neoplasms of the eyelid); disruption of the formation of the tear film (insufficient tear fluid in keratoconjunctivitis sicca, insufficient secretion of conjunctival goblet cells); infection (in cats, most often herpesvirus); congenital anomalies (epithelial basement membrane disease, endothelial dystrophy, etc.), others (foreign body, chemical burns, neurotrophic keratitis, immunopathological diseases). One of the causes of corneal ulcers is lagophthalmos (failure to close the eyelids), leading to the development of exposure keratitis and dry eye. It occurs in brachycephalic dog breeds, and is often observed with exophthalmos, buphthalmos, or the neuroparalytic form of idiopathic facial paralysis (especially in cocker spaniels).
Diagnostics
Ulcerative keratitis can be acute or chronic. The owner of the animal notices lacrimation, squinting, and redness of the eye. A history of trauma sometimes reveals a respiratory disorder in cats with herpetic keratitis.
Nonspecific signs of eye disease are noted: serous or serous-purulent discharge, blepharospasm, photophobia, conjunctival hyperemia. On examination, the cornea reveals one or more round, linear, or geographic (i.e., map-like) defects. A crater-shaped defect is characteristic of a deep ulcer of the corneal stroma and descemetocele. Depending on the size, cause of the ulcer and duration of the disease, neovascularization (ingrowth of blood vessels), pigmentation, edema, scarring of salt or lipid deposits, infiltration, enzymatic melting of the corneal stroma (foci of opacification) are also possible. Refractory (slow-healing) ulcers have jagged or redundant edges; When stained with fluorescein, the dye is retained in areas of seemingly intact epithelium.
A corneal ulcer stimulates the formation of tear fluid, resulting in intense lacrimation (tears sometimes flood the face). The absence of lacrimation raises suspicion of keratoconjunctivitis sicca.
Ulcerative keratitis is sometimes accompanied by “reflex” anterior uveitis, which is manifested by miosis, decreased intraocular pressure (compared to a healthy eye), and effusion in the anterior chamber.
Differential diagnosis is carried out with other causes of red eye syndrome (conjunctivitis, keratoconjunctivitis sicca, uveitis and glaucoma). The most informative study is with fluorescein staining.
LABORATORY AND OTHER RESEARCH METHODS
Clinical and biochemical blood and urine tests are usually within normal limits. To confirm a herpetic infection, a serological test is performed (diagnostic titers > 1:100), but its negative results do not exclude the disease.
To detect erosion and ulcers, a study with fluorescein is performed. With superficial and deep ulcers, the damaged area of the cornea is uniformly colored green. Its depth is assessed subjectively. In descemetocele, fluorescein accumulates at the periphery of the crater-shaped ulcer, and its center is not stained. If the dye is poorly retained in the crater-shaped defect and easily flows out of it, a healed ulcer should be assumed. Rose Bengal staining reveals superficial linear (tree-like) ulcers, pathognomonic of feline herpetic ulcerative keratitis.
For deep or rapidly progressing ulcers, a bacteriological study is necessary to determine the sensitivity of the microflora to antibiotics. Bacteriological examination of corneal scrapings with Gram, Giemsa and Wright stains may be useful. The Schirmer test is used to confirm keratoconjunctivitis sicca.
Treatment
Animals with deep or rapidly progressing corneal ulcers are hospitalized. If the defect is deep or there is a descemetocele, in order to prevent perforation of the cornea, it is necessary to limit physical activity. To prevent the animal from damaging its eyes, a special collar is worn.
Antibiotics are prescribed locally for ulcers of any etiology. Ointments provide a longer duration of contact of the drug with the cornea; they are placed in the conjunctival sac every 6-12 hours. Solutions are instilled more often (4-8 times a day). The most common drugs are chloramphenicol, terramycin (a combination drug containing oxytetracycline and polymyxin B), erythromycin, gentamicin and tobramycin. At the initial stages of treatment, the combination of neomycin, polymyxin B and bacitracin is considered the best, providing activity against a wide range of microorganisms. Gentamicin and tobramycin (and fluoroquinolones if resistant to them) are prescribed for rapidly progressing ulcers, suspected keratitis caused by Pseudomonas aeruginosa and other gram-negative microorganisms.
Atropine (1% ointment or solution) is used in the treatment of “reflex” anterior uveitis. The drug is prescribed every 8-24 hours, gradually reducing the dose.
Antiviral drugs are prescribed for feline herpetic ulcerative keratitis. Solutions of trifluridine or idoxuridine are instilled every 4-6 hours until clinical improvement, after which the frequency of administration is gradually (over 1-2 weeks) reduced.
Anticollagenolytic agents. Acetylcysteine is most often used in the treatment of corrosive ulcers, but its effectiveness is not undisputed. A 20% solution is diluted to a concentration of 5-10% with artificial tear fluid and instilled every 2-4 hours.
The drug can also be mixed with antibiotics: 5 ml of 20% acetylcysteine solution, 2 ml of gentamicin solution for injection (50 mg in 1 ml) are diluted in 8 ml of artificial tear fluid.
NSAIDs have anti-inflammatory and analgesic activity. Aspirin is prescribed orally to dogs at a dose of 10-15 mg/kg every 12 hours; cats 10 mg/kg every 48 hours.
When several medications are prescribed simultaneously, at least 5 minutes should pass between the installations of each of them.
Contact lenses protect the cornea from irritation, reduce pain and retain medications. Lenses find their greatest use in the treatment of refractory ulcers, remaining an alternative or complement to surgical treatment. Disadvantages include their relatively high cost ($13-15) and the possibility of displacement from the cornea. In veterinary practice, lenses of various diameters (13.5-17.0 mm) and curvature (8.5-9.0 mm) are used.
Contraindications. Local corticosteroids are contraindicated for corneal erosions and ulcers, NSAIDs for herpetic ulcerative keratitis, atropine for glaucoma and lens luxation. For ulcers caused by herpes viruses and canine distemper, cyclosporine should not be prescribed topically.
Atropine suppresses the production of tear fluid, so it is prescribed with caution to animals with keratoconjunctivitis sicca. NSAIDs (flubiprofen, diclofenac) and corticosteroids slow down ulcer healing.
Superficial ulcers are usually treated conservatively.
In some cases, surgery can eliminate the cause of ulcerative keratitis (correction of entropion, removal of a foreign body, etc.). Indications for surgery are also an ulcer that extends to more than half the thickness of the cornea, descemetocele, and ineffectiveness of drug treatment. If the cornea is perforated, its integrity must be immediately restored.
Refractory (slow-healing) ulcers under superficial anesthesia are treated with a dry sterile swab, and uneven epithelial edges are removed. Surgical treatment methods include puncture or mesh keratotomy, superficial keratectomy, and conjunctival flap transplantation. Most authors recommend rotational pedicled conjunctival flap grafting.
Follow-up
Monitoring of ulcer healing is carried out by periodic examination of the affected eye with fluorescein staining. Typically, surface defects close in 3-5 days. Slow healing indicates that the cause of the ulcer has not been eliminated or that the animal has a disease of the epithelial basement membrane. In the latter case, treatment is carried out according to the principles of refractory ulcer therapy. Deep ulcers affecting the stroma of the cornea and rapidly progressing ulcers at the initial stage of treatment are examined every 1-2 days until improvement or arrest of development.
To prevent ulcerative keratitis in brachycephalic dog breeds, moisturizing ointments (lubricants) are prescribed and/or partial tarsography is performed. For dry keratoconjunctivitis, a parotid duct transplant is performed. To prevent recurrence of herpetic ulcers, long-term constant or course antiviral therapy is carried out.
Possible complications: corneal perforation, endophthalmitis, secondary glaucoma, blindness. For vision loss and chronic pain, enucleation is sometimes used.
Course of the disease and prognosis: uncomplicated superficial ulcers usually heal within 5-7 days (1 mm per day). The healing process of refractory ulcers, despite therapy, sometimes drags on for up to several weeks or even months. Deep ulcers extending into the stroma close within a few weeks. However, there is a possibility of incomplete healing, as well as the development of complications (perforation). After surgical closure of the defect with a conjunctival flap, improvement occurs within a few days.